In Memoriam: John B. Robbins, M.D.
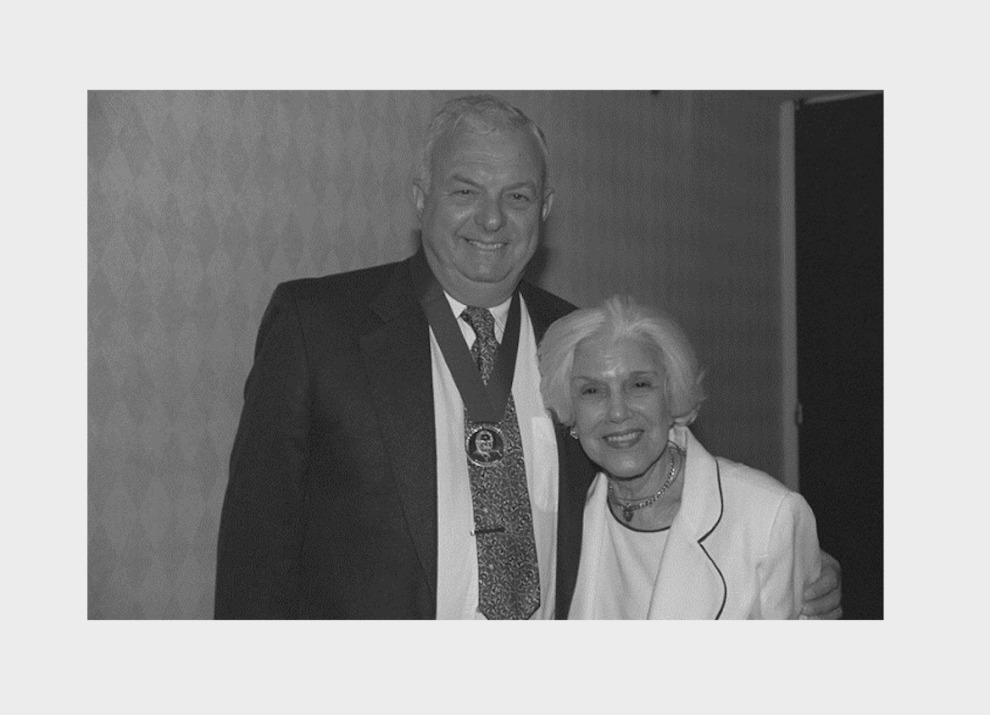
Dr. John B. Robbins died on November 27, 2019 at age 86. Dr. Robbins was the 2001 recipient of the Sabin Gold Medal for his pivotal role in the development of Hib conjugate vaccine, which is now used throughout the world. The use of this vaccine led to a dramatic decline in the number of infants and children suffering from meningitis and other systematic infections such as osteomyelitis and pneumonia. He continued his work into his 70s, serving as Chief of the Laboratory of Developmental and Molecular Immunity, National Institutes of Child Health and Human Development at the National Institutes of Health for nearly 30 years. He also played an important role in the development of vaccines for typhoid fever, pertussis and many others. Below is the text of the speech he delivered on April 23, 2001 when he accepted the Sabin Gold Medal.
I would like to express thanks to the Committee, recognition to my family and Rachel, special thanks to my colleagues at the Laboratory of Developmental and Molecular Immunity, National Institutes of Health, the Center for Biologics Evaluation and Research and Centers for Disease Control including Louis D. Rodrigues, J.C. Parke, Osmar Barrera, Ann Sutton, William Egan, and Willie Vann. In addition, I wish to thank our special gurus: Meir Wilchek, Porter Anderson, Robert Austrian and Emil C. Gotschlich.
Not commonly known was that Dr. Sabin was elected to the National Academy of Sciences before he developed poliovirus vaccine, based upon his work on dengue fever and toxoplasmosis. Albert Sabin was also a president of the United Bialystockers, an organization of immigrants and refugees from Bialystock, Poland that collected money to bring friends and relatives from their town to the United States. Fund raising was difficult in those years, because most immigrants from eastern Europe were poor and their kinsmen in Poland were in precarious condition.
The formalin-inactivated poliovirus vaccine developed by Salk and his colleagues, licensed in 1954, induced less than optimal immunity, and production was marginal. Sabin’s orally-administered vaccine became available in 1965. Routine vaccination with the attenuated poliovirus was soon implemented in the US, Canada, and most of the developed countries in the late 1960s. But, paralytic polio continued to occur in most of Central and South America, Africa, and Southeast Asia. The inability to vaccinate all children against polio was blamed largely upon the limited personnel and funds available to public health programs. Stimulated by the failure of many developing countries to achieve universal polio vaccination, Sabin campaigned for concentrating resources by supplementing public health personnel with volunteers, to focus nation-wide publicity to a short period each year.
This approach was successful in several countries including Brazil and Cuba. In the late 1980s, Sabin’s scheme was adopted by the Pan American Health Organization under the direction of Dr. Ciro de Quadros, who received the Sabin Gold Medal Award last year for eliminating wild-type poliovirus from the Americas. Sabin’s approach to eliminating poliovirus infection was ultimately adopted in the 1990s. Although delayed by conflicts in parts of Africa and Asia, elimination of paralytic polio will be achieved, but only about half a century after polio vaccine became available. Notable was the fact that the World Health Organization initially opposed Mass Polio Vaccination Days, stating that these could interfere with existing routine vaccination programs. The success of Polio Mass Vaccination strengthened rather than weakened programs for immunization of children. As it has been said, “Nothing smells sweeter than the sweet smell of success.”
My remarks tonight are not directed towards the development of Haemophilus influenzae type b conjugate–its successes are well known. My best recollections about those years are the wonderful people I met and the help and advice given to Rachel and me by our colleagues. Rather than dwell on old hat, I will speak about a current problem of vaccination that shames our profession – – that of group A meningococcal meningitis in Africa. My presumption in presenting this topic was stimulated by the experience of Dr. Albert Sabin and his colleagues in bringing polio vaccine to all children.
Dr. Rachel Schneerson of our Laboratory and Dr. Emil C. Gotschlich of the Rockefeller University and I have encountered similar inertia on the part of the World Health Organization, to recommend routine immunization against endemic and epidemic group A meningococcal meningitis in the “meningitis belt” of Africa. Their recommendation for epidemic control only is based upon distortions of both the immunologic data and clinical experience with group A polysaccharide, and is claimed to be justified by the slightly different schedule required for group A polysaccharide vaccine, which would compromise existing programs.
Meningococci are capsulated: three capsular polysaccharides denoted as group antigens, A, B, and C comprise most of the cases. Each has unique immunologic properties that distinguish them from all other medically important bacterial polysaccharides. Group A meningococci have caused epidemics throughout the world during the past century. Unlike any other polysaccharide, Group A induces a booster response between 3 months and 2 years of age. This regime induced protective levels of antibodies and prevented meningitis in infants and young children in Finland and New Zealand. Groups B and C cause endemic meningitis and occasionally acute and protracted outbreaks. Group B polysaccharide is non-immunogenic. Group C polysaccharide does not induce protective antibody levels up to the age of 2 years, and reinjection induces suppression in this age group. In older children and young adults, a single injection of groups A, C, W135 and Y polysaccharides elicits a protective serum antibody response that is probably lifelong.
The problem of epidemic group A meningococcal meningitis has been described by the WHO. Reported cases of meningococcal disease in African countries in the 10 year period 1988 – 1997 total 704,000, a figure which is likely to be a significant underestimate of the true number. About 100,000 people have died as a result of the disease during this period. In 1996, an epidemic involving more than 180,000 reported cases took place, the largest epidemic ever recorded. Epidemics on this scale cannot be ignored. In addition to epidemics, group A meningococci regularly cause about 30,000 cases of meningitis annually. This “endemic” rate is considered epidemic in industrialized countries. The mortality is at least 10 percent. At least 30 percent of “cured” patients, even under optimal conditions, suffer permanent central nervous system damage including impairment or loss of hearing, mental retardation, seizures, and blindness. Despite antibiotics and other supportive therapy, meningococcal meningitis remains a serious disease. Obviously, prevention is preferred to treatment.
To combat this terrible problem, the WHO strategy attempts to predict an epidemic by detecting the number of meningitis cases to be >15/100,000 per week for two weeks in several villages. When this information is confirmed, mass vaccination is initiated with one injection of bivalent groups A and C meningococcal polysaccharide vaccine to the “at-risk” population. This sentinel strategy failed to prevent the worst recorded epidemic of group A meningococcal meningitis in 1996. Again in 1997, Sudan endured an epidemic of 32,000 cases and 2,200 deaths, and Ghana of 18,703 cases and about 1,400 deaths. The WHO vaccination campaign in Ghana was tardy, despite five weeks of warning from an epidemic in adjacent Togo. Had mass vaccination in Ghana started 6 months earlier, there would have been no epidemic. But even with optimal detection and mobilization of personnel and resources, all authorities agree that at best, the WHO strategy will prevent only 50% of cases during an epidemic.
We and African workers have proposed that mass vaccination of the entire population, followed by routine vaccination of infants with group A polysaccharide will prevent both epidemic and endemic meningococcal meningitis. Two examples are cited.
First, vaccination with group A polysaccharide was started in 3 northern provinces of Benin, with about 50 percent coverage between 1993 and 1996. During that period, Benin had no epidemics in this area, whereas neighboring Burkina Faso and Togo suffered epidemics in 1996 and 1997. Second are the severe epidemics of group A meningococcal meningitis which were reported in China in 1957, 1966, and 1976. Thereafter, routine vaccination of infants and school children was initiated in 1980. Since then there have been relatively few cases and no epidemics. The situation was different in adjacent Mongolia. As in China, in 1976 a severe epidemic in Mongolia was halted by a trial of group A polysaccharide vaccine. But there was no follow-through of immunization. Mongolia experienced a severe epidemic in 1995 through 1997, with an overall attack rate of 1 percent. Only after the worst part of the epidemic occurred did the WHO initiate mass vaccination.
The keystone of the WHO’s failure to recommend this safe, stable, inexpensive, available, and highly effective vaccine for routine vaccination is justified largely in a report in the Lancet, July 20th, 1985. Because it is so pivotal to the discussion, I summarize this report and urge all of you to read it.
The West African country of Burkina Faso has endured epidemics about every 8 to 12 years throughout the 20th century. During the first 3 months of 1981, 3,800 cases of group A meningococcus meningitis were reported. This prompted wide-scale vaccination with one dose of bivalent group A and C vaccine; about 103,000 children were vaccinated. In its capital city, approximately 48,000 children, between the ages of 7 and 12 years were vaccinated or approximately 98 percent of children who were in school. Approximately 45 percent of the estimated 55,000 younger children between the ages of 3 months and 6 years were vaccinated once. Because of logistical constraints, vaccination cards were given to only some of the vaccinees, making future evaluation of the vaccine’s effect difficult. In 1983, another 25,000 doses were given mainly to unvaccinated school children. Incomplete records were kept, because the number of vaccinees is expressed as approximate in thousands rather than in exact numbers.
The nature of and who conducted the surveillance is not described. About half of the confirmed cases in the capital’s main hospital were discarded from the analysis.
There were no serologic studies.
In 1982, one year after the main vaccination program, the CDC evaluated the efficacy of the vaccine using a case control method.
Three years after vaccination, the efficacy was 92 percent in the 4 to 7 year-olds and 75 percent in the 8 to 16 year-olds: the difference between the age groups was not statistically significant. As expected from the extensive studies of group A polysaccharide, the efficacy in 1 to 3 year-olds after one year was 89 percent, which declined to about 22 percent after three years.
Several aspects of this report should be mentioned. First, there was no comment on the usefulness of the vaccine for the 5 to 16 year-olds, the very age group with the highest attack rate of meningitis in this and all other epidemics in Africa. Second, the authors failed to mention that the package insert recommended that two injections, spaced several months apart, should be given during 3 month to 2 years of age, with an additional booster about one year later. The authors’ conclusion about the limited degree and extent of immunity conferred by one injection of group A meningococcal polysaccharide to infants and young children, therefore, is invalid. Would we discuss the immunity to diphtheria, tetanus, and pertussis conferred by one injection of DTP? Of course not!
Lastly, the authors state, “Although routine vaccination of children at four years of age might increase the duration of protection and hence might have an impact on this pattern of disease, the cost and logistic problems involved in instituting such a programme may be prohibitive.” The authors state that a group A meningococcal polysaccharide conjugate vaccine is needed for routine vaccination of Africa. We can hardly be accused of ignoring the potential of polysaccharide conjugate vaccine. But a conjugate will not be widely available for at least five years, its cost will be considerably higher than the polysaccharide, and as with all conjugates, it must be administered more than once during the first year of life. Thus, conjugates will increase the cost of routine vaccination against group A meningococcal meningitis compared to that of the polysaccharide alone. What will the WHO do then?
This article describes the hasty response of a nation reacting to epidemic meningococcal meningitis by mass vaccination and not a scientifically designed and meticulously executed study. This study certainly should not be used to formulate an international policy for prevention of this serious, poorly treated, and common disease. Nevertheless, the authors extracted data from this trial that showed a high level of efficacy in older children and a rate of protection for infants and children that, as predicted from previous data, declined rapidly. Our conclusions from this study are exactly opposite from those drawn by the WHO–group A meningococcal polysaccharide, when administered as directed, would be an effective method for preventing both endemic and epidemic group A meningococcal meningitis. The recommendation that group A meningococcal polysaccharide should be used for epidemic control only is not based upon sound data, experience, or logic. It is based upon what the WHO and CDC think can be done, rather than on what should be done.
Although there are as yet only incomplete data, in January and April of this year, severe outbreaks in Ethiopia, Sudan, Benin, Burkina Faso, Cameroon, Chad, Nigeria, and Niger have been reported – another epidemic may have occurred this year.
During the next five years, at least 125,000 African children will contract group A meningococcal meningitis if there is only endemic disease – the number could double or triple if there is an epidemic. Without exception, data from all over the world gathered over the past 25 years allows the prediction that endemic and epidemic meningococcal meningitis in Africa can be prevented now by mass vaccination followed by routine vaccination with group A meningococcal polysaccharide vaccine.
Our plea is simple. Dr. Albert Sabin’s experience with the WHO should not be lost. We urge the vaccine community and those interested in the care of African children to read the references on this subject and to urge the Director of the WHO to review and reconsider her failed program. With such a review, we predict that the WHO will recommend prevention by routine vaccination rather than the control of epidemic meningitis.
Since Dr. Robbins made this appeal, the meningococcal prevention landscape has transformed dramatically. Starting in 2001, PATH, WHO and Serum Institute of India partnered to develop MenAfriVac, the first vaccine to be developed specifically for Africa. MenAfriVac, a meningococcal group A conjugate vaccine that provides longer-lasting protection than its polysaccharide predecessors, was rolled out in 2010 through mass immunization campaigns at a price of $.50 per dose. The vaccine has been incredibly effective, with one study finding a 60 percent decline in meningitis cases among vaccinated populations. Per WHO’s updated recommendation of including group A meningococcal vaccine in routine immunization, MenAfriVac is now being introduced into routine immunization programs across the meningitis belt.